Orthopaedic physicians use a variety of diagnostic tests to help identify the specific nature of musculoskeletal injuries or conditions. Orthopaedists also use results of these tests to plan an appropriate course of treatment. Here are some of the most frequently used diagnostic tests for musculoskeletal injuries and conditions.
Radiographs (X-rays)
X-rays (radiographs) are the most common and widely available diagnostic imaging technique. Even if you just complain about a sprain in your wrist or ankle, your doctor will probably order radiographs to make sure no bone is broken. X-rays are always used for fractures and joint dislocations, and may also be recommended if your doctor suspects damage to a bone or joint from other conditions such as arthritis or osteonecrosis (bone cell death). The part of your body being pictured is positioned between the X-ray machine and photographic film. As you hold still, the machine briefly sends electromagnetic waves (radiation) through your body. This exposes the film, creating a picture of your internal structure. The level of radiation exposure from X-rays is minimal, but your doctor will take special precautions if you are pregnant. Bones, tumors and other dense matter appear white or light because they absorb the radiation. Soft tissues and breaks in bone let radiation pass through, making these parts look darker. Several X-rays from different angles may be needed. If you have a fracture in one limb, your doctor may want a comparison X-ray of your uninjured limb. Your X-ray session will probably take 10 to 15 minutes; no specific preparations are required.
Magnetic Resonance Imaging (MRI)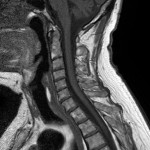
An MRI (magnetic resonance image) uses magnetic fields and a sophisticated computer to take high-resolution pictures of your bones and soft tissues, resulting in a cross-sectional image of your body. It can be used to help diagnose torn muscles, ligaments and cartilage, heriated disks, hip or pelvic problems and other conditions. The patient lies on a table that slides into the tube-shaped MRI scanner. The MRI creates a magnetic field around, then pulses radio waves to the area of the body to be pictured. The radio waves cause tissues to resonate. A computer records the rate at which your body’s various parts (tendons, ligaments, nerves) give off these vibrations, and translates the data into a detailed, two-dimensional picture. There is no pain while undergoing an MRI, but the machine may be noisy. An MRI takes 30 to 90 minutes, and is not available at all hospitals.
Computed Tomography (CT Scan)
A CT scan (computed tomography) combines X-rays with computer technology to produce a more detailed, cross-sectional image of your body. It may be ordered if your doctor suspects a tumor or a frature that doesn’t appear on X-rays (such as in your collarbone or pelvis) or if you’ve had severe trauma to the chest, abdomen, pelvis or spinal cord. The process is painless. You lie motionless on a table as it slides into the center of the cylinder-like CT scanner. An X-ray tube slowly rotates around you, taking many pictures from all directions. A computer combines the images to produce a clear, two-dimensional view on a television screen. You may need to drink or be injected with barium sulfate or a dye so that certain parts of your body can be seen more clearly. Tell your doctor if you are pregnant before undergoing a CT scan.
Discography
Discography is a test used to determine whether the discs, the cushioning pads that separate the bones of the spine, are the source of back pain. It may be performed before surgery to positively identify the painful disc(s) or to determine which particular disc is causing the pain, so that another non-surgical treatmant option can be used. Before the procedure begins, you will be given antibiotics and relaxation medications through an IV line. Medication is used to numb the skin over the test site. During the procedure, the doctor inserts a needle into one or more discs and injects a contrast dye. You’ll feel pain when the dye is introduced into the problem disc. Afterward, a CT scan will show any changes in the disc size or shape. You may experience some muscle discomfort after the procedure; your doctor can prescribe pain relievers to ease the discomfort.
Electromyography (EMG) and Nerve Conduction Studies (NCS)
EMG & NCS are done together to determine if a nerve is functioning normally. It may be recommended if you have symptoms of carpal tunnel syndrome or ulnar nerve entrapment, or have back or neck pain with numbness and tingling into the extremities. The doctor conducting the test will tape wires (electrodes) to the skin in various places along the nerve pathway. Then the doctor stimulates the nerve with an electric current. As the current travels down the nerve pathway, the electrodes placed along the way capture the signal and measure its speed. In healthy nerves, electrical signals can travel at speeds of up to 120 miles per hour. If the nerve is damaged, however, the signal will be slower and weaker. By stimulating the nerve at various places, the doctor can determine the specific site of the injury. Nerve conduction studies also may be used during treatment to test the progress being made. Although you may initially be startled by the suddenness of the stimulation, it is not usually painful and most people are comfortable during the testing procedure. The shock is similar to one received when you touch a doorknob after walking across carpeting.
An electromyography (EMG) records and analyzes the electrical activity in your muscles. It is used to learn more about the functioning of nerves in the arms and legs. For example, a fracture of the upper arm bone (humerus) may tear or pinch the radial nerve. An EMG can be used to identify the damage if nerve function doesn’t return within 3 months of the injury. During an EMG, small, thin needles are placed in the muscle to record the electrical activity. When the needles are inserted, you may feel some pain and discomfort. The doctor will ask you to relax the muscle and then to tense it slightly. The electrical signals generated by your muscle are broadcast on a TV-like screen. When the needles are removed, you may experience some soreness and bruising, but this will disappear in a few days. There are no long-term side effects. If you are taking blood-thinning medications, have lung disease or are at risk for infection, tell the physician who is conducting the test. On the day of the test, do not put any lotions or creams on the area to be tested and do not wear any jewelry. Usually, you can get the results immediately after the test.
Bone Scan
Two very different kinds of tests may be called bone scans. One type tests the density of the bone and is used to diagnose osteoporosis. This type of bone scan uses narrow X-ray beams or ultrasound to see how solid the bone is. No preparation is required for this test, which takes only a few minutes and has no side effects. (See Dual-Photon Absorptiometry, Dual-Energy X-ray Absorptiometry, and Peripheral Bone Density Testing.)
The second type of bone scan is used to identify areas where there is unusually active bone formation. It is frequently used to pinpoint stress fracture sites or the presence of arthritis, infection, or cancer. About three hours before the scan, you will be given a dose of a mildly radioactive substance called “technetium” through an intravenous line (IV). This substance occurs naturally in your body and is used in the bone formation process. The bone scan itself is performed about three hours later, which gives the bone time to absorb the technetium. As you lie on a table, a special nuclear camera takes a picture of your entire body. This process takes 30 to 90 minutes. Areas of abnormal bone formation activity will appear brighter than the rest of the skeleton. No fasting or other preparation is required. The amount of radioactivity absorbed during a technetium bone scan is minimal, and there are usually no side effects. You may feel some discomfort as the IV line is placed. Some people may feel nauseous. Tell your physician if you are or may be pregnant or are a nursing mother before you schedule this test.
Blood Tests
As part of your examination, your orthopaedist may order a variety of blood tests. Some conditions, such as rheumatoid arthritis, may be identified by the presence of a specific substance in your blood. You may be asked to fast prior to the exam. Usually a blood test is a simple matter that involves withdrawing a small amount of blood from your arm.
Non-Surgical Orthopaedics, P.C. specializes in the non-surgical treatment of orthopaedic injuries. Please call 770-421-1420 for more information or visit our website at www.lowbackpain.com.
